What everyone should know about bulimia nervosa. Causes, treatment

[author] [author_image timthumb='on']https://buildyourbody.org/wp-content/uploads/2020/08/Nataniel-Josue-Alvarez.jpg[/author_image] [author_info]The article was reviewed and approved by Nataniel Josue Alvarez. Medical Doctor graduated from Medical School Universidad Nacional Experimental Francisco de Miranda. Área Ciencias de la Salud.[/author_info] [/author]
Some people binge on food beyond satiety. They then vomit, take medication, or exercise excessively to prevent weight gain.
This behavior is known as bulimia nervosa. It is one of three eating disorders described in the Diagnostic and Statistical Manual of Mental Disorders along with anorexia nervosa and binge eating disorder. These eating disorders are associated with a wide range of psychiatric and somatic illnesses.
Bulimia nervosa is a very complex disorder without a specific pathophysiological origin. It often affects young people in Western countries in particular. It has a significant impact on the gastrointestinal, nutritional, and mental spheres, not to mention the social consequences it entails.

The prevalence of bulimia nervosa is 0.28%. The rate of episodes is about 3 cases per 100,000 people.
Unfortunately, doctors reported incidences of up to 300 per 100,000 population to have among adolescents and young women between 16 and 20 years of age.
Sadly, the age of onset of this disorder is declining, with patients as young as nine years old.
What is bulimia? Symptoms of Bulimia Nervosa

Bulimia nervosa is a severe eating disorder with some fatal potential.
Its main sign is the intake of a large amount of food in a short time, followed by practices that seek to prevent weight gain.
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, published in 2015, they describe Bulimia Nervosa as:
- Recurrent episodes of binge eating. These episodes usually last less than 2 hours. They occur at least once a week for three consecutive months. The amount of food is significantly more than any individual needs. Lack of control during these episodes
- Compensatory behaviors to prevent weight gain. Self-induced vomiting. Inappropriate use of laxatives, diuretics, or other medications. Excessive exercise. Prolonged fasting
- Impaired vision of body shape and weight.
The patient's reporting usually makes the diagnosis of bulimia nervosa of symptoms.
Unlike anorexia, there are no apparent signs of weight loss. The person with Bulimia knows that he or she is hurting himself or herself and that his or her behavior is harmful.
Unfortunately, embarrassment and wanting to keep the disease a secret prevents the disclosure of symptoms and delays the start of treatment.
Bulimia nervosa goes with other mental illnesses, such as mood and anxiety disorders.
Of particular concern is the high incidence of suicide among young people with this eating disorder.
The rate of autolysis is higher than in anorexia nervosa.
More than half (53%) of adolescents diagnosed with bulimia nervosa have ever considered suicide. Also, more than one-quarter of them (17%) have made one or more attempts.
Causes of Bulimia
Although the term Bulimia was recently coined - in 1979 by the English psychiatrist Gerald Russell - its study dates back much further.
Thanks to these studies, it is now known that this disorder may have several combined causes, including:
- Hormonal disturbances. Cholecystokinin. Oxytocin
- Intestinal disturbances. Disorders of the intestinal microbiota
- Genetic factors.
- Combination of the above.
Hormonal alterations
We can find the reason for this disorder in a hormone deficiency. Cholecystokinin is a hormone produced in the intestine when fatty foods pass from the stomach to the duodenum, where bile helps process this fat.
While this digestive process takes place, the stomach does not empty, maintaining the feeling of fullness longer and inhibiting the desire to eat.
When there is a deficit of cholecystokinin, the stomach goes empty faster, and the person feels hungry early and urgently.
They believe that cholecystokinin acts directly on the hunger and thirst centers at the level of the brain, thus boosting the appetite when the hormone is lacking.
There is evidence of reduced food intake when this hormone is administered exogenously to experimental animals and humans.
Some clinical trials have tested cholecystokinin levels in normal-weight people with Bulimia and compared them with healthy people.
The results show lower values of this substance in people with Bulimia.
Treatment with external cholecystokinin seems promising. So do some antidepressants that help raise levels of the hormone mentioned above.
Another hormone that may be related to the incidence of Bulimia is oxytocin.
This neurohormone is related to food intake. It is also related to the emotional, cognitive, and social functioning of the individual.
While we can find no significant differences in oxytocin levels in healthy people compared to bulimic patients, there is evidence of clinical improvement following the administration of exogenous oxytocin.
Intestinal disturbances
The intestinal microbiota, or the usual presence of some bacteria in the intestine, plays a fundamental role in the systems:
- Immunology.
- Gastrointestinal.
- Endocrinological.
- Mental.
These bacteria also contribute to the physiological regulation of the appetite. They can modify the sensation of fullness and satiety.
The molecular nature of this mechanism is not entirely known. Some metabolites produced by this microbiota seem to mimic several of the hormones that regulate satiety.
Also, they seem to influence the behavior of certain neurotransmitters of central action, such as dopamine and serotonin.
These play an essential role in the satiation feeling. Dopamine and serotonin have linked its alteration for decades to the genesis of bulimia nervosa.
Genetic Factors
As for many other diseases, several genetic studies are being conducted around the world to try to link eating disorders to a genetic disorder.
For now, despite limited data, the results look promising.
There are recent pathophysiological studies on the origin of bulimia nervosa. They speak of a combination of genetic, environmental, nutritional, immunological, and endocrine causes to explain this disorder.
Those studies associated with the primary genetic defects of bulimia nervosa have implications for the individual's digestive processes.
From hormonal deficits to dysfunctions of the organs of the gastrointestinal tract, we can see all the alterations in Bulimia Nervosa have some related genetic defects.
Consequences of Bulimia Nervosa
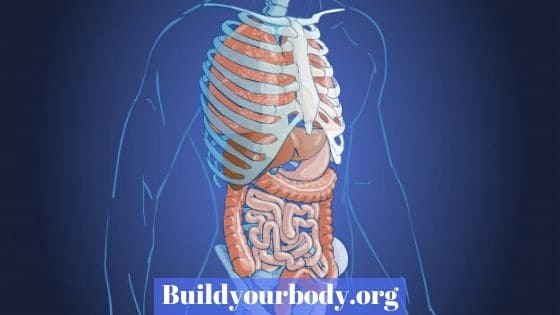
The multifactorial origin of this disease has many consequences in the body from a medical point of view. Among the systems most affected by bulimia nervosa are:
Gastrointestinal system
- Boca
- Esophagus
- Stomach
- Intestines
Cardiorespiratory system
- Bronchial aspiration
- Pneumothorax or pneumomediastinum
- Cardiac arrhythmias
Endocrine system
- Menstrual alterations
- Decreased blood potassium
Mental sphere
- Anxiety
- Altered body image
- Depression
- Migraine
Most of these complications are associated with self-induced vomiting.
From the mouth, with an increased incidence of mucous membranes and tooth decay, to esophageal and stomach perforations, gastrointestinal symptoms are the most common.
The vomit can lead to respiratory distress — besides, lung infections, and even pneumothorax or pneumomediastinum.
Bulimic patients tend to suffer from depression and anxiety. These pathologies are the first to be treated so that the others do not appear.
Physicians often focus on managing mental disorders through psychotherapy.
Some menstrual disorders can be seen in women with Bulimia as a result of hormonal problems.
The decreased caloric intake from recurrent vomiting can compromise an individual's weight and overall health.
However, the body's vision is not as altered as in patients with anorexia, although there is still an abnormal perception of the body.
Treatment for Bulimia Nervosa
Bulimia nervosa, like almost all eating disorders and psychiatric disorders, has a multifactorial therapeutic approach. The management of bulimia nervosa includes:
- Non-pharmacological treatment. Cognitive-behavioral therapy. Interpersonal therapy. Cognitive-affective therapy. Psychodynamic therapy. Supportive Psychotherapy.
- Pharmacological treatment. Antidepressants. Fluoxetine. Trazodone.
- Other drugs.
- Hormones. Cholecystokinin. Oxytocin. Oestrogens.
Non-pharmacological treatment
Cognitive-behavioral therapy

Cognitive-behavioral therapy is the mainstay of psychological treatment for both adolescents and adults with bulimia nervosa.
It helps patients to understand that their illness has a significant mental component and that if they can manage it, their symptoms will improve substantially.
Interpersonal therapy

Sometimes bulimic and anorexic patients are treated together.
These group therapies are useful to exchange experiences, alternative therapies, and to make friends.
This type of treatment is called "interpersonal therapy" or "symptom exchange," and the results are positive.
Family members or people close to you can also participate in these meetings, which is especially useful for adolescents and young people.
Cognitive-affective therapy
The participation of loved ones in psychotherapy sessions is increasingly accepted and encouraged.
This treatment not only provides basic psychoeducation about Bulimia but also guides the family in their role in restoring regular eating practices.
The family and cognitive-affective therapy, group, and individual sessions allow us to know how the family nucleus works as a whole and the patient individually.
Psychodynamic therapy

The psychodynamic therapy tries to make the patient assume some characteristics of his illness that so far are unconscious and, in this way, try to give them a solution or at least control them.
Although it is not easy to explain or understand, we can summarize psychodynamic therapy in the knowledge of the true self of each patient to understand their problems.
Sometimes these sessions are conducted without the presence of the therapist or in an "empty chair" to stimulate self-analysis.
Supportive Psychotherapy
When people finally understand the mental component of their eating disorder, psychotherapeutic treatment is much more comfortable.
From that point on, they only need supportive therapy, with short, less intense sessions, to help maintain the person's mental stability.
Pharmacological treatment
Antidepressants
The doctors that treat patients with bulimia nervosa, maybe:
- Psychiatrists.
- Internists.
- Gastroenterologists
These usually indicate medication to complement psychotherapy, especially in those cases that are difficult to manage.
The most commonly used drugs are antipsychotics or antidepressants, such as fluoxetine.
Several clinical trials conducted in adults and adolescents combined a daily dose of fluoxetine of 60 mg with cognitive therapy.
The medication was well-tolerated, and all participants maintained their treatment throughout the weeks of the study.
All of these trials showed decreases in the number of binges and compensatory behaviors.
However, discontinuation of medication brought a worsening of bulimic symptoms
Trazodone is an FDA-approved antidepressant for the treatment of major depression.
However, among its non-depressant uses is Bulimia.
An initial dose of 50 mg appears to have positive effects on the patient with eating disorders. Sleepiness and sedation associated with its use may compromise its administration.
Other drugs
They are studying an alternative Bulimia treatment — anti-epileptic drugs such as topiramate and zonisamide.
The same is true for an opioid antagonist, naltrexone. Naltrexone has been shown in recent years to be useful in the management of certain eating disorders.
What happens when combined with other medications and psychological therapy.
Hormones
As mentioned above, hormone therapy has been successful in the management of bulimia nervosa.
The administration of exogenous cholecystokinin showed a decrease in the incidence of binge eating and prevented self-induced vomiting and diarrhea. Thus, it became a real therapeutic alternative for this disorder.
However, cholecystokinin is not a commonly used drug and is not readily available in any pharmacy.
There is only a freeze-dried powder presentation of 75 units. Its approved use is for diagnostic studies of gastrointestinal diseases, such as pancreatic and hepatic disorders, and not for therapeutic purposes.
It does not indicate treatment for any disease by the FDA.
Oxytocin is much more readily available but does not have approval for use in the management of Bulimia.
Remember that exogenous oxytocin is used primarily as a labor inducer or accelerator, to control postpartum uterine bleeding, and for assessment of fetal respiratory capacity as part of the fetal reactivity test.
In experimental animals, oxytocin administered directly to the brain attenuates food intake and reduces body weight.
In humans, intranasal oxytocin has shown promising effects in the management of anorexia. There are as yet no significant studies to justify its use in Bulimia.
We believe that alterations in serotonin may play an essential role in the pathophysiology of bulimia nervosa.
Many women with Bulimia have high levels of testosterone. This hormone is predominantly male, which decreases the central uptake of serotonin
To counteract the effects of testosterone, these patients were given birth control pills with high estrogen content.
They reduced symptoms of Bulimia, as were other associated signs.
However, further studies are needed to verify these results as data are currently very scarce.
Anorexia and Bulimia
The main difference between anorexia and Bulimia is the significant weight loss that exists in the former and is not common in the latter.
Remember that in anorexia, there is a real restriction in caloric intake. That is due to an altered perception of one's body, which makes the patient feel and looks obese.
In Bulimia, we don't see our body altered. For other reasons, the person eats large amounts of food compulsively.
Prevention

Bulimia nervosa is an eating disorder whose importance has not yet been assumed by the scientific world.
It seems to be more of a social problem than a medical one, and this assessment is far from the truth.
The worst part of the problem is that the affected population is often the youngest and least likely to seek help.
That is why prevention is the most important thing, and the family plays a fundamental role in this task.
- When we detect signs of insecurity or low self-esteem in a family member, we have to provide immediate support.
- We have to promote a balanced diet in case of overweight, and the virtues of the committed family member should be enhanced.
- Also, we must make people understand that body shape is not an essential thing in life. Also, we must not believe everything that appears in social networks and media concerning physical appearance.
Environmental factors are the easiest to modify to prevent Bulimia.
Paragraph
The work or study site should be friendly, without the presence of multimedia elements that could be disturbing.
Finally, information is essential. We have to know the problem; its complications and treatment can help prevent it.
You can find more interesting articles like this in our health section.
[author] [author_image timthumb='on']https://buildyourbody.org/wp-content/uploads/2020/08/Nataniel-Josue-Alvarez.jpg[/author_image] [author_info]Article reviewed and approved by Dr. Nataniel Josué Alvarez. Medical Doctor graduated from Medical School Universidad Nacional Experimental Francisco de Miranda Área Ciencias de la Salud. •Awarded winner IV Science Fair of Research Methodology - April 2012 •Recipient of Asesor Estudiantil Institucional Scholarship •Thesis: Relationship Between Parasitosis, Anemia and Hygiene Habits in patients aged 20 yo 70 years old in Amuay, municipality of Los Taques, Falcón State, Venezuela •Thesis: Intervention Plan in Rural Healthcare in Monte Verde and La Puntica sectors, of the Amuay Community, Los Taques parish, Los Taques municipality, of the Falcón State, Venezuela. During the period March 2018 - July 2018[/author_info] [/author]